The emergence of COVID-19 has caused hospitals around the world to face unprecedented strain and put the spotlight on healthcare sectors globally. Effective management and prevention of infectious diseases become significant, with focus placed on healthcare facilities that can achieve “Infection Control”. A key component of infection control includes having infectious disease control facilities that are designed with good medical planning, and with safe mechanical systems implemented within the premises. Coupled with a strict set of medical SOPs and good medical teams, infection control can be accomplished.
In our previous blog post “Designing Healthcare Facilities for Infectious Diseases: Part 1- Medical Planning”, we discussed how good medical planning can strengthen an infectious disease facility’s capacity to isolate and treat patients with different types of infectious diseases. Here, let’s look at how safety designs in mechanical systems help protect the occupants in a healthcare facility.
While protective measures and Personal Protective Equipment (PPE) are essential for ensuring the well-being of the medical team, mechanical systems act as vital organs to a health facility, providing fresh air, water and other important elements that keep the facility running efficiently and safely. Thus, whether the air-conditioning and mechanical ventilation (ACMV) systems, as well as waste management control systems are designed for use safely, is paramount to the prevention of nosocomial infections (infections contracted in the health facility).
Air flow and Air Pressure Management Designs
Majority of nosocomial infections are caused by factors such as poor hygiene practice, and surface-to-surface contamination, however there are some risks of infections that spread via AC systems. The designs of AC systems within an infectious health facility are thus motivated with a desire to reduce infections via air transmission.
(i) Air change rate and Dilution
One method of reducing the time or number of microbes to which a person is exposed is by increasing the dilution rate of clean air into a space. For instance, when our CPG mechanical engineering team was working on the National Centre for Infectious Diseases (NCID) project, the air in the patient rooms are constantly purged with a rate of minimum 12 times the room volume per hour (12 ACH). This air setting reduces the exposure time of microorganisms generated within the room and dilutes the air for the safety of the medical staff and patients.
(ii) Air movement and Pressure Regime
Pressure relationship helps in mitigating the spread of infections. Within healthcare facilities, many rooms require various pressure relative to adjacent spaces. The intent of pressurisation is to move potentially infectious particles from the cleanest areas to less clean areas. It is important that the rooms are designed with negative pressure. That means the supply from the Air Handling Units (AHU), which is used to re-condition and circulate air as part of the air-conditioning system, is less than the air exhaust from the room; creating a minimum negative pressure of -2.5 Pa from the ward corridors. In this way, the air inside the patient room would not flow out into the corridor. To facilitate the movement of the medical staff into the room, an ante room is provided. The inner and outer doors are interlocked such that only one door would open at any one time. This minimises the air movement by keeping opened channels to a minimum.
For more complicated layouts, such as the High Level Isolation Units (HLIU) and Operating Theatres, the pressures for adjacent rooms and interlocking of doors have to be considered carefully to ensure that contaminated air does not flow to the cleaner areas.
While the basic requirements do not seem complicated, the implementation and design of a ward with, say, 15 or more patient rooms with supporting facilities would require substantial detailing and design considerations. To control the correct amount of air entering each room, normal VAV (variable air volume) control is not sufficiently accurate. Instead, venturi valves which help create constriction in pipes to vary the flow characteristic of air are used to control the flow rates of the air supply and exhaust.
With the movement of medical staff through the ante rooms and other operation rooms, air pressure changes. The venturi valves, which control the air supply and exhaust, constantly adjust to maintain the air flow and pressure requirements.
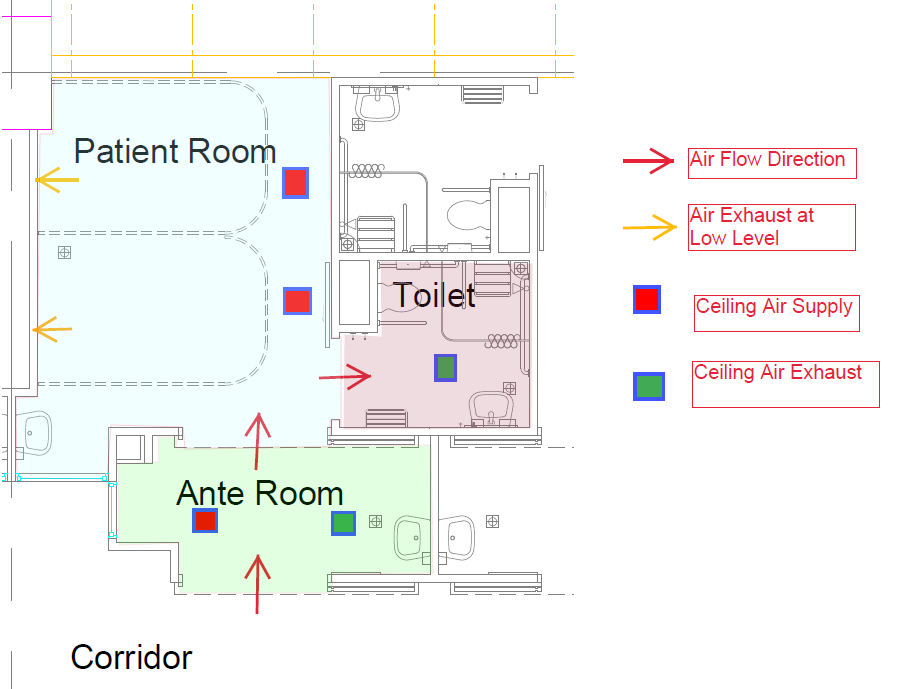
Diagram: Air Flow through a patient room
Within the patient room, the air is supplied from the ceiling near the foot of the patient bed. The air exhaust is at a lower level near the head of the bed. In this way, the contaminated air from the patient is removed as soon as possible and the medical staff is better protected with clean air.
To maintain the comfort and quality levels of the air-conditioning, the temperature and humidity levels are targeted at 24 ±1oC and 55+-5% respectively. The AHUs are provided with coils which first cool then heat, to meet the temperature and humidity based on psychometrics calculations. Heat pumps are provided to save heating energy, which is substantial for the air flow involved.
The safety of the areas around the wards cannot be neglected either. In fact, the exhaust air from the ward rooms has to be treated using the High Efficiency Particulate Air (HEPA) filter. As an added safety measure, UV lights are also provided. The air is then exhausted out by high plume fans, to further dilute and jet the exhaust air into the atmosphere above the roof.
Other than patient rooms, the infectious diseases facility also includes other amenities used to treat and administer checks on infectious patients. These include operation theatres and radiology centres, etc. In the case of more serious outbreaks, screening centres and clinics housed within the facility are available to manage the potentially larger number of patients. It is important that the air flow and pressure regime in these areas are controlled. Especially in supporting facilities such as laboratories where samples from the infectious patients are drawn and tested, the air flow and pressure regime in each of these areas have to be tailored to meet the layout and operation requirements, while preventing contamination.
An example is the operating theatre. Pressure regimes are required to manage air flow between the operating theatre, the patient preparation room and the scrub room. In usual cases, the design is such that the air will flow outwards to the corridor. This differs however in a situation where infection control is needed. In the case of an infectious diseases facility, the air in the supporting rooms around the operating theatre would have to be let out via air exhaust ducts, so that contaminated air will not flow to the corridors, patient and staff area outside the operating theatre suite, contributing to infection control.
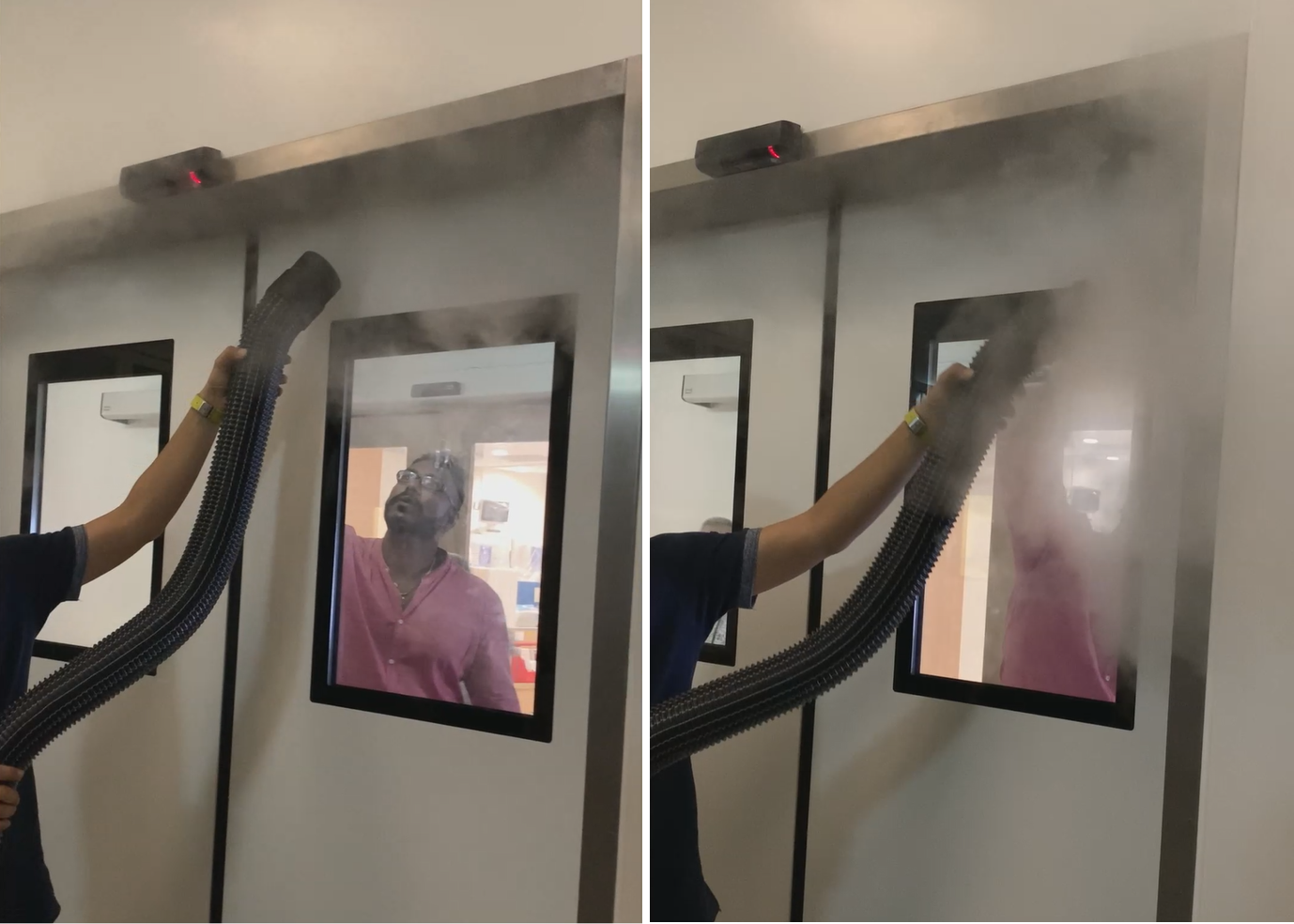
Testing of the Operation Theatre ensuring that contaminated air does not flow out
When implementing air flow and pressure regime designs, it is important to ensure that everything is based on design calculation. Even during the construction stage, the rooms have to be tested for air tightness to make sure that the settings are in accordance to calculation. The air tightness includes the walls, the floor and the soffit as well as the pipe, ducts and wiring into the rooms.
For the testing and commissioning of the completed installation, besides the usual operation tests, failure modes of the systems are also checked and fine-tuned. For example, if an AHU or High Plume Fan fails, it may cause contaminated air to flow out from the patient rooms and into the clean areas. Thus, mitigation measures are devised for each failure scenario, including the anticipation of control network failure. Failure scenarios are also tested for other areas such as laboratories, clinics which require infection control.
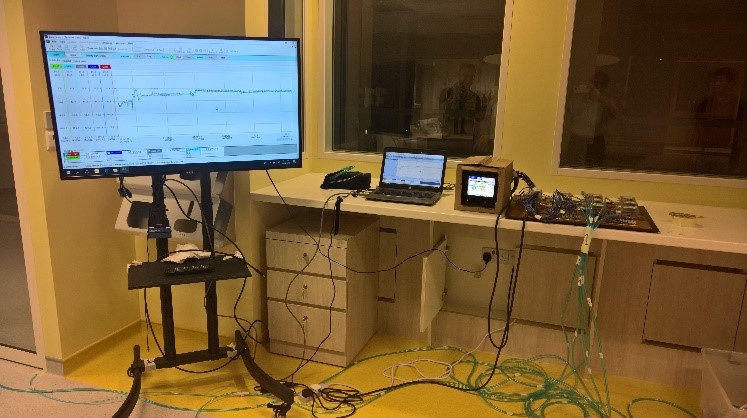
Failure Scenario Test in the Ward
Sanitary Waste Management

Sanitary Disinfection Plant
Conclusion
This blog post is the second part of a two-part series introducing CPG Consultants’ experience with specialised healthcare facilities designed to handle infectious diseases.
Covid-19 has transformed much of the way we live. How can our built environment be more pandemic-resilient?
Read more at our special section for insights on a pandemic-resilient BE by our multi-disciplinary experts.
This article was authored by:
Ar. Patrick Lam, Senior Consultant
Architecture Group, CPG Consultants Pte. Ltd


